Courses

ACNE
Director: Jerry Tan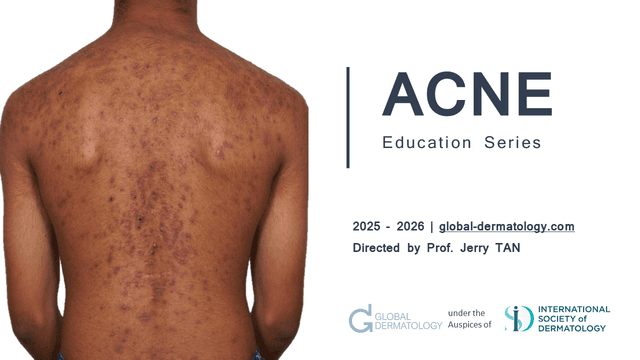
The ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.

DERMOSCOPY
Director: Awatef Kelati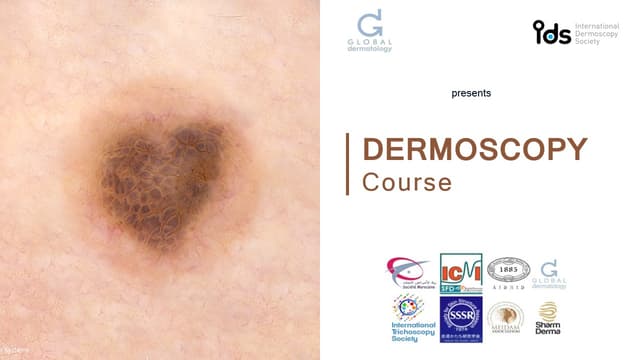
This comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.

CYSPERA MEDICAL EDUCATION
Director: Global Dermatology
Cyspera® is a topical pigment-correcting treatment formulated with cysteamine, a naturally occurring compound that reduces the appearance of persistent hyperpigmentation, including melasma, post-inflammatory hyperpigmentation, and lentigines. It is known for being non-hydroquinone, suitable for long-term use, and effective on all skin types.

PIGMENTATION
Director: Seemal Desai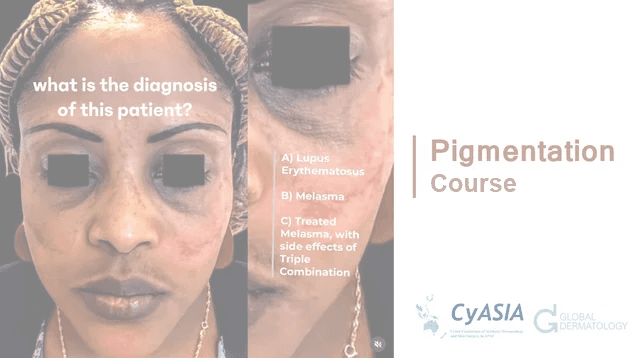
Hyperpigmentation is excess skin color from melanin. Understand melanin synthesis mechanisms and main causes.

PSYCHODERMATOLOGY
Director: Mohammad Jafferany
This specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.

TOPOGRAPHIC DERMOSCOPY
Director: Awatef Kelati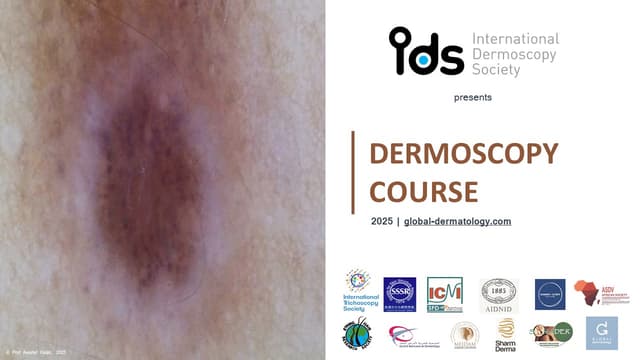
Topographic dermoscopy refers to the region-specific application of dermoscopic examination, emphasizing the unique morphological patterns found across different anatomical sites. On facial skin, the dermoscopic assessment requires recognizing patterns influenced by the high density of pilosebaceous units and sun-induced changes, often presenting pseudonetworks and annular-granular structures. The ear, with its thin skin and sebaceous gland concentration, reveals specific vascular and follicular clues important in distinguishing benign from malignant lesions.
On the chest and back, where the skin is thicker and sun exposure varies, dermoscopy must account for irregular pigment distribution and architectural disorder, especially in large nevi or early melanomas. Limb lesions may show distinctive features due to mechanical friction, hair density, and vascular variations, demanding precise interpretation to identify atypical nevi or skin cancers.
Palmar and plantar dermoscopy highlights the parallel ridge pattern critical for melanoma diagnosis, contrasting with benign acral patterns like the parallel furrow or lattice-like structures. Scalp and hair disorders benefit from trichoscopy, where dermoscopic evaluation reveals specific signs such as yellow dots, broken hairs, or black dots, aiding in the diagnosis of alopecia areata, androgenetic alopecia, or tinea capitis.
In nail disorders, onychoscopy enables visualization of melanonychia, hemorrhages, and nail matrix changes, crucial for distinguishing subungual melanoma from benign causes like trauma or fungal infection. Mucosal dermoscopy, though technically challenging, provides diagnostic clues in pigmented lesions of the lips, genitalia, or oral mucosa, requiring adaptation to moist, non-keratinized surfaces.
Finally, ultraviolet dermoscopy reveals a unique application: scabies mites fluorescing bright green under UV light, enhancing detection when traditional visualization fails. Topographic dermoscopy thus demands both anatomical knowledge and technical adaptation to maximize diagnostic accuracy across diverse body sites.

NEGLECTED TROPICAL SKIN DISEASES
Director: Prajwal Pudasaini
Neglected tropical skin diseases affect poor populations in tropical areas. They include leprosy, mycetoma, and cutaneous leishmaniasis, causing disability and stigma. They receive little attention and resources, leading to poor diagnosis and treatment. Increased awareness and improved healthcare access are needed to help affected communities.

ACNE TREATMENT IN CHINA
Director: Haiping Zhang
Acne treatment in China combines traditional methods with modern practices.

CUTANEOUS MEDICINE: MULTIDISCIPLINARY APPROACHES IN DERMATOLOGY
Director: Fahafahantsoa Rapelanoro Rabenja
This course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.

TROPICAL DERMATOLOGY AND NEGLECTED TROPICAL DERMATOSES
Director: Fahafahantsoa Rapelanoro Rabenja.jpg&w=640&q=75)
Dermatological diseases, particularly neglected tropical diseases (NTDs) with skin manifestations like deep mycosis (chromoblastomycosis, sporotrichosis, mycetoma), scabies, leprosy, lymphatic filariasis, and cutaneous leishmaniasis, pose major challenges for healthcare systems in resource-limited regions of Africa, Asia, and Latin America. These conditions severely affect vulnerable populations, suffering from frequent underdiagnosis and inadequate treatment that exacerbates suffering. Diseases such as atopic dermatitis are also under consideration for inclusion as skin NTDs through collaborative efforts involving ISAD, ASDV, and WHO. Furthermore, albinism, highly prevalent in sub-Saharan Africa, presents significant social challenges including stigmatization and occult beliefs. Despite these complex difficulties, the field is undergoing a historic transformation driven by science and technology, particularly artificial intelligence (AI), which offers tangible tools for improving diagnosis, treatment, and prevention. The participation of global experts facilitates vital knowledge exchange, exploration of innovative solutions, and helps address critical shortages of human and material resources in remote areas.
Learning Objective:
Understand the complex challenges posed by dermatological diseases, especially skin NTDs and conditions like albinism, in resource-limited settings, and recognize the critical role of global collaboration, technological innovation (particularly AI), and expert knowledge exchange in developing solutions to improve diagnosis, treatment, prevention, and resource allocation.
Education Modules
ACNE | EPIDEMIOLOGY AND BURDEN
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
SPONSORED PRESENTATION | GALDERMA
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
SPONSORED PRESENTATION | EUCERIN
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
SPONSORED PRESENTATIONS
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
ACNE PATHOPHYSIOLOGY
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
ACNE MANAGEMENT
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
ACNE TREATMENT IN CHINA
ACNEThe ACNE | Education Series, led by Dr. Jerry Tan, is a comprehensive global medical education initiative designed to enhance the understanding and skills of dermatologists and healthcare practitioners regarding acne. Participants will gain insights from leading international experts on the latest advancements in acne research, innovative treatment options, and patient-centered care approaches. The event features interactive discussions, live Q&A sessions, and evidence-based strategies, all at no cost. The esteemed faculty includes specialists from the USA, Italy, France, the UK, Singapore, Greece, Australia, Canada, and Germany. This is a valuable opportunity to improve clinical competencies and stay updated on current acne management practices.
Attendees will acquire up-to-date knowledge on acne pathophysiology, new therapeutic options, and patient-oriented management strategies to optimize clinical outcomes in acne treatment. The session will also provide practical insights through expert-led discussions and evidence-based approaches.
DERMOSCOPY FOR EVERYONE BY THE IDS
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
DERMOSCOPY SKIN OF COLOR
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
DERMOSCOPY IN GENERAL DERMATOLOGY
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
DERMOSCOPY | DIAGNOSIS OF SKIN CANCER
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
DERMOSCOPY IN PIGMENTED LESIONS
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
TOPOGRAPHIC DERMOSCOPY
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
MY BEST CASES OF THE YEAR WORLDWIDE - PART 1
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
MY BEST CASES OF THE YEAR WORLDWIDE - PART 2
DermoscopyThis comprehensive dermoscopy course provides dermatologists and healthcare professionals with essential skills in skin lesion evaluation, covering fundamental principles through advanced diagnostic applications across five key areas: global dermoscopy practices, pigmented lesion analysis (including differentiation of benign and malignant patterns), specialized techniques for skin of color, skin cancer detection (melanoma and non-melanoma), and general dermatological conditions (inflammatory, infectious, and hair/nail disorders). Participants will develop proficiency in recognizing diagnostic patterns, adapting techniques for diverse skin types, and applying dermoscopic algorithms, ultimately enhancing their clinical accuracy through a combination of theoretical knowledge and practical case-based learning. The course emphasizes real-world application, addressing both common and challenging scenarios in dermatological practice.
CYSPERA MEDICAL EDUCATION
Cyspera Medical EducationCyspera® is a topical pigment-correcting treatment formulated with cysteamine, a naturally occurring compound that reduces the appearance of persistent hyperpigmentation, including melasma, post-inflammatory hyperpigmentation, and lentigines. It is known for being non-hydroquinone, suitable for long-term use, and effective on all skin types.
PANEL DISCUSSION
Cyspera Medical EducationCyspera® is a topical pigment-correcting treatment formulated with cysteamine, a naturally occurring compound that reduces the appearance of persistent hyperpigmentation, including melasma, post-inflammatory hyperpigmentation, and lentigines. It is known for being non-hydroquinone, suitable for long-term use, and effective on all skin types.
HYPERPIGMENTATION
PigmentationHyperpigmentation is excess skin color from melanin. Understand melanin synthesis mechanisms and main causes.
PSYCHODERMATOLOGY IN COSMETIC DERMATOLOGY
PsychodermatologyThis specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.
PSYCHIATRIC DISEASES IN DERMATOLOGY
PsychodermatologyThis specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.
MANAGEMENT OF DERMATOLOGICAL DELUSIONAL DISORDERS
PsychodermatologyThis specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.
MENTAL HEALTH IN CHRONIC DERMATOSES
PsychodermatologyThis specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.
BODY DYSMORPHIC DISORDER AND ZOOM DYSMORPHIA
PsychodermatologyThis specialized course explores the vital intersection between dermatology and mental health, equipping clinicians with the knowledge and tools to manage psychodermatological conditions effectively. Through a blend of theoretical knowledge and practical application, participants will learn to diagnose and treat dermatological delusional disorders, identify psychiatric comorbidities in skin disease patients, and implement mental health strategies for chronic dermatoses. The curriculum also examines psychological factors in cosmetic dermatology and provides cutting-edge screening techniques for body dysmorphic disorder, including modern digital manifestations like Zoom dysmorphia. Adopting a patient-centered approach, the course emphasizes multidisciplinary management of conditions where psychological and dermatological factors interact. Participants will gain expertise in recognizing psychiatric components of skin diseases, addressing the emotional
burden of chronic conditions, and applying ethical principles in cosmetic practice. The training combines expert instruction with case-based learning to bridge theory and clinical practice. Designed for dermatologists, psychiatrists, psychologists, and primary care providers, this program enhances clinicians' ability to deliver holistic care that addresses both the visible and invisible aspects of skin disorders. Upon completion, practitioners will be better prepared to manage complex psychodermatological cases while improving patient outcomes through integrated mind-skin healthcare.
TOPOGRAPHIC DERMOSCOPY
Topographic DermoscopyTopographic dermoscopy refers to the region-specific application of dermoscopic examination, emphasizing the unique morphological patterns found across different anatomical sites. On facial skin, the dermoscopic assessment requires recognizing patterns influenced by the high density of pilosebaceous units and sun-induced changes, often presenting pseudonetworks and annular-granular structures. The ear, with its thin skin and sebaceous gland concentration, reveals specific vascular and follicular clues important in distinguishing benign from malignant lesions.
On the chest and back, where the skin is thicker and sun exposure varies, dermoscopy must account for irregular pigment distribution and architectural disorder, especially in large nevi or early melanomas. Limb lesions may show distinctive features due to mechanical friction, hair density, and vascular variations, demanding precise interpretation to identify atypical nevi or skin cancers.
Palmar and plantar dermoscopy highlights the parallel ridge pattern critical for melanoma diagnosis, contrasting with benign acral patterns like the parallel furrow or lattice-like structures. Scalp and hair disorders benefit from trichoscopy, where dermoscopic evaluation reveals specific signs such as yellow dots, broken hairs, or black dots, aiding in the diagnosis of alopecia areata, androgenetic alopecia, or tinea capitis.
In nail disorders, onychoscopy enables visualization of melanonychia, hemorrhages, and nail matrix changes, crucial for distinguishing subungual melanoma from benign causes like trauma or fungal infection. Mucosal dermoscopy, though technically challenging, provides diagnostic clues in pigmented lesions of the lips, genitalia, or oral mucosa, requiring adaptation to moist, non-keratinized surfaces.
Finally, ultraviolet dermoscopy reveals a unique application: scabies mites fluorescing bright green under UV light, enhancing detection when traditional visualization fails. Topographic dermoscopy thus demands both anatomical knowledge and technical adaptation to maximize diagnostic accuracy across diverse body sites.
NEGLECTED TROPICAL SKIN DISEASES
Neglected Tropical Skin DiseasesNeglected tropical skin diseases affect poor populations in tropical areas. They include leprosy, mycetoma, and cutaneous leishmaniasis, causing disability and stigma. They receive little attention and resources, leading to poor diagnosis and treatment. Increased awareness and improved healthcare access are needed to help affected communities.
ACNE TREATMENT IN CHINA
Acne Treatment in ChinaAcne treatment in China combines traditional methods with modern practices.
ATOPIC DERMATITIS AND ALLERGOLOGY
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
HYPERPIGMENTATION
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
MENTAL HEALTH IN CHRONIC DERMATOSES
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
DERMOSCOPY IN PIGMENTED LESIONS
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
DERMOSCOPY SKIN OF COLOR
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
NEGLECTED TROPICAL SKIN DISEASES
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
PSYCHODERMATOLOGY IN COSMETIC DERMATOLOGY
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
HAIR DISORDERS MANAGEMENT
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
This course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
DERMOSCOPY IN GENERAL DERMATOLOGY
Cutaneous Medicine: Multidisciplinary Approaches in DermatologyThis course explores the intersection of dermatology with other medical specialties, emphasizing a collaborative approach to diagnosing and managing complex skin disorders. It covers a wide range of topics, including dermatopathology, rheumatology, oncology, and infectious diseases, highlighting how systemic conditions manifest cutaneously. With contributions from experts in various fields, the text provides comprehensive insights into multidisciplinary care, advanced diagnostic techniques, and innovative treatments. Ideal for dermatologists, internists, and specialists, it bridges gaps between disciplines to improve patient outcomes in cutaneous medicine.
PEDIATRIC DERMATOLOGY
Tropical Dermatology and Neglected Tropical DermatosesDermatological diseases, particularly neglected tropical diseases (NTDs) with skin manifestations like deep mycosis (chromoblastomycosis, sporotrichosis, mycetoma), scabies, leprosy, lymphatic filariasis, and cutaneous leishmaniasis, pose major challenges for healthcare systems in resource-limited regions of Africa, Asia, and Latin America. These conditions severely affect vulnerable populations, suffering from frequent underdiagnosis and inadequate treatment that exacerbates suffering. Diseases such as atopic dermatitis are also under consideration for inclusion as skin NTDs through collaborative efforts involving ISAD, ASDV, and WHO. Furthermore, albinism, highly prevalent in sub-Saharan Africa, presents significant social challenges including stigmatization and occult beliefs. Despite these complex difficulties, the field is undergoing a historic transformation driven by science and technology, particularly artificial intelligence (AI), which offers tangible tools for improving diagnosis, treatment, and prevention. The participation of global experts facilitates vital knowledge exchange, exploration of innovative solutions, and helps address critical shortages of human and material resources in remote areas.
Learning Objective:
Understand the complex challenges posed by dermatological diseases, especially skin NTDs and conditions like albinism, in resource-limited settings, and recognize the critical role of global collaboration, technological innovation (particularly AI), and expert knowledge exchange in developing solutions to improve diagnosis, treatment, prevention, and resource allocation.
ATOPIC DERMATITIS
Tropical Dermatology and Neglected Tropical DermatosesDermatological diseases, particularly neglected tropical diseases (NTDs) with skin manifestations like deep mycosis (chromoblastomycosis, sporotrichosis, mycetoma), scabies, leprosy, lymphatic filariasis, and cutaneous leishmaniasis, pose major challenges for healthcare systems in resource-limited regions of Africa, Asia, and Latin America. These conditions severely affect vulnerable populations, suffering from frequent underdiagnosis and inadequate treatment that exacerbates suffering. Diseases such as atopic dermatitis are also under consideration for inclusion as skin NTDs through collaborative efforts involving ISAD, ASDV, and WHO. Furthermore, albinism, highly prevalent in sub-Saharan Africa, presents significant social challenges including stigmatization and occult beliefs. Despite these complex difficulties, the field is undergoing a historic transformation driven by science and technology, particularly artificial intelligence (AI), which offers tangible tools for improving diagnosis, treatment, and prevention. The participation of global experts facilitates vital knowledge exchange, exploration of innovative solutions, and helps address critical shortages of human and material resources in remote areas.
Learning Objective:
Understand the complex challenges posed by dermatological diseases, especially skin NTDs and conditions like albinism, in resource-limited settings, and recognize the critical role of global collaboration, technological innovation (particularly AI), and expert knowledge exchange in developing solutions to improve diagnosis, treatment, prevention, and resource allocation.
INFECTIOUS DERMATOLOGY
Tropical Dermatology and Neglected Tropical DermatosesDermatological diseases, particularly neglected tropical diseases (NTDs) with skin manifestations like deep mycosis (chromoblastomycosis, sporotrichosis, mycetoma), scabies, leprosy, lymphatic filariasis, and cutaneous leishmaniasis, pose major challenges for healthcare systems in resource-limited regions of Africa, Asia, and Latin America. These conditions severely affect vulnerable populations, suffering from frequent underdiagnosis and inadequate treatment that exacerbates suffering. Diseases such as atopic dermatitis are also under consideration for inclusion as skin NTDs through collaborative efforts involving ISAD, ASDV, and WHO. Furthermore, albinism, highly prevalent in sub-Saharan Africa, presents significant social challenges including stigmatization and occult beliefs. Despite these complex difficulties, the field is undergoing a historic transformation driven by science and technology, particularly artificial intelligence (AI), which offers tangible tools for improving diagnosis, treatment, and prevention. The participation of global experts facilitates vital knowledge exchange, exploration of innovative solutions, and helps address critical shortages of human and material resources in remote areas.
Learning Objective:
Understand the complex challenges posed by dermatological diseases, especially skin NTDs and conditions like albinism, in resource-limited settings, and recognize the critical role of global collaboration, technological innovation (particularly AI), and expert knowledge exchange in developing solutions to improve diagnosis, treatment, prevention, and resource allocation.
PSYCHODERMATOLOGY
Tropical Dermatology and Neglected Tropical DermatosesDermatological diseases, particularly neglected tropical diseases (NTDs) with skin manifestations like deep mycosis (chromoblastomycosis, sporotrichosis, mycetoma), scabies, leprosy, lymphatic filariasis, and cutaneous leishmaniasis, pose major challenges for healthcare systems in resource-limited regions of Africa, Asia, and Latin America. These conditions severely affect vulnerable populations, suffering from frequent underdiagnosis and inadequate treatment that exacerbates suffering. Diseases such as atopic dermatitis are also under consideration for inclusion as skin NTDs through collaborative efforts involving ISAD, ASDV, and WHO. Furthermore, albinism, highly prevalent in sub-Saharan Africa, presents significant social challenges including stigmatization and occult beliefs. Despite these complex difficulties, the field is undergoing a historic transformation driven by science and technology, particularly artificial intelligence (AI), which offers tangible tools for improving diagnosis, treatment, and prevention. The participation of global experts facilitates vital knowledge exchange, exploration of innovative solutions, and helps address critical shortages of human and material resources in remote areas.
Learning Objective:
Understand the complex challenges posed by dermatological diseases, especially skin NTDs and conditions like albinism, in resource-limited settings, and recognize the critical role of global collaboration, technological innovation (particularly AI), and expert knowledge exchange in developing solutions to improve diagnosis, treatment, prevention, and resource allocation.
